Mental Illness Awareness Week – Starting the Conversation

With Mental Illness Awareness Week upon us from October 3rd – 9th, followed by World Mental Health Day on October 10th, there’s never been a better time to educate yourself and others about the importance of mental health. That includes checking in on friends and family who may be suffering and starting important conversations.
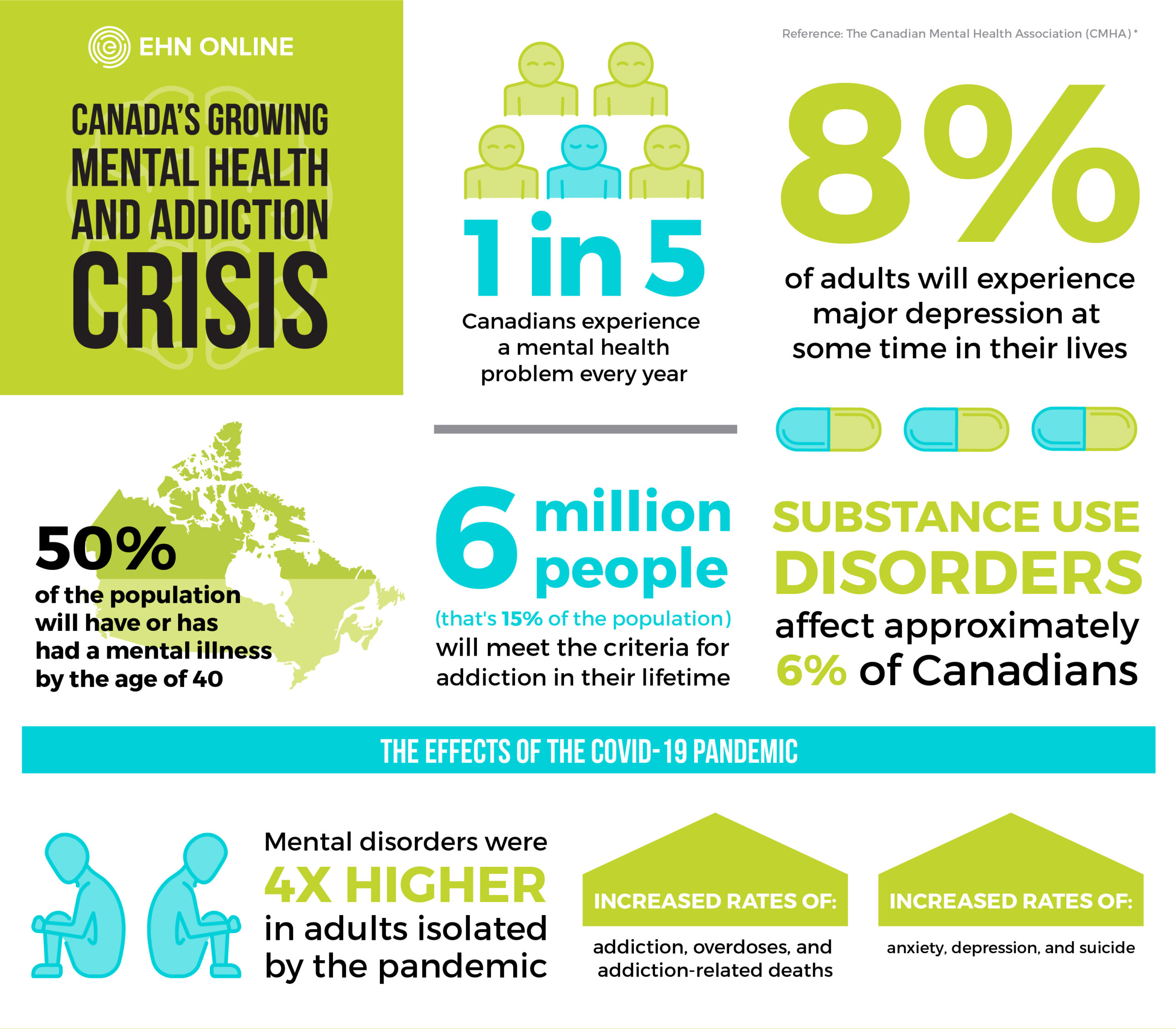
Oftentimes, people don’t seek out the treatment they need in the early stages as they don’t recognize the symptoms. October 3rd begins a week of national reckoning about the breadth of mental disorders, how they can be treated and how we can help stop the stigma still sadly associated with them. Mental Illness Awareness Week not only brings some much-needed attention to these devastating disorders, it aims to help people understand the symptoms so they can get the help they need. Considering 1 in 3 Canadians will experience mental illness during their lifetime, this is something that simply cannot be ignored.
The 8 most common types of mental health conditions
Whether occasional or chronic, there are many different types of mental health conditions with many different symptoms. Here are some of the most common types:
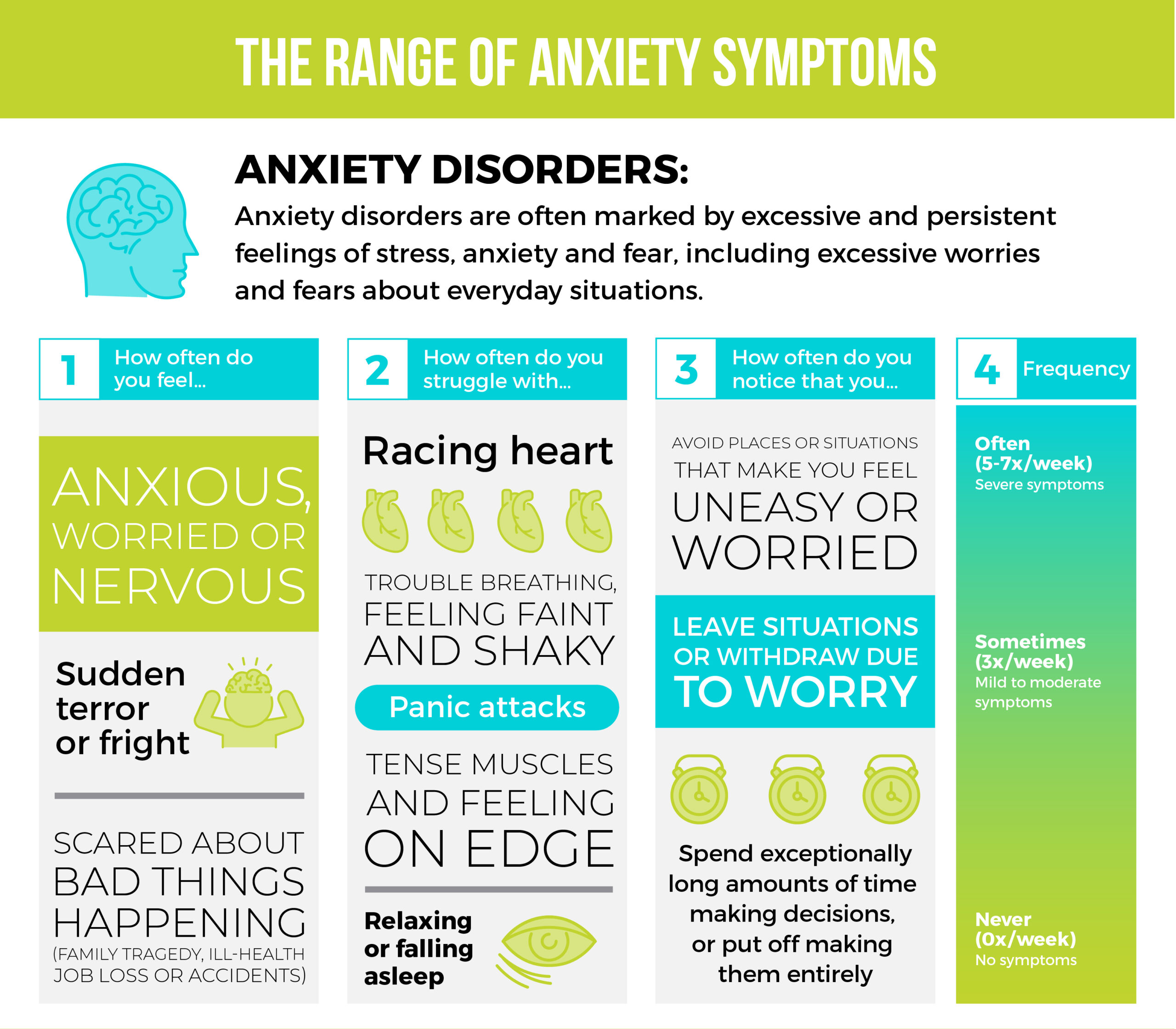
Anxiety – We’ve all experienced anxiety, whether before an important test, presentation or life event. An anxiety disorder on the other hand, is an illness that causes people to feel frightened, distressed or uneasy for no apparent reason. This type of anxiety can seriously interfere with a person’s quality of life, affecting their sleeping and eating patterns, and in severe cases, their ability to function through life.
Bipolar Disorder – This mental health disorder is characterized by extreme highs and lows in mood and energy, beyond regular mood swings. Everyone experiences ups and downs in life, but people with bipolar disorder experience them at higher frequency and severity. The shifts that occur within this condition are severe and can seriously impact a person’s life, causing major disruption within the family. They can even affect a person’s ability to hold down a job.
Schizophrenia – People who suffer from this challenging disorder have a difficult time distinguishing between what’s real and what’s isn’t. They may see or hear things that aren’t there (hallucinations) or have unusual ideas or views that aren’t shared by others (delusions). They also have a hard time thinking clearly, managing emotions, relating to others and functioning normally, which typically causes them to act out in confusion or fear.
Eating Disorders – Those struggling with an eating disorder often become obsessed with food, body image and/or weight. One of the most common types is bulimia nervosa, characterized by periods of binge eating and then purging with laxatives or vomiting. The other is anorexia nervosa, when people avoid food completely or severely restrict their intake. Both conditions can lead to serious health issues, such as heart and kidney problems, or sometimes death.
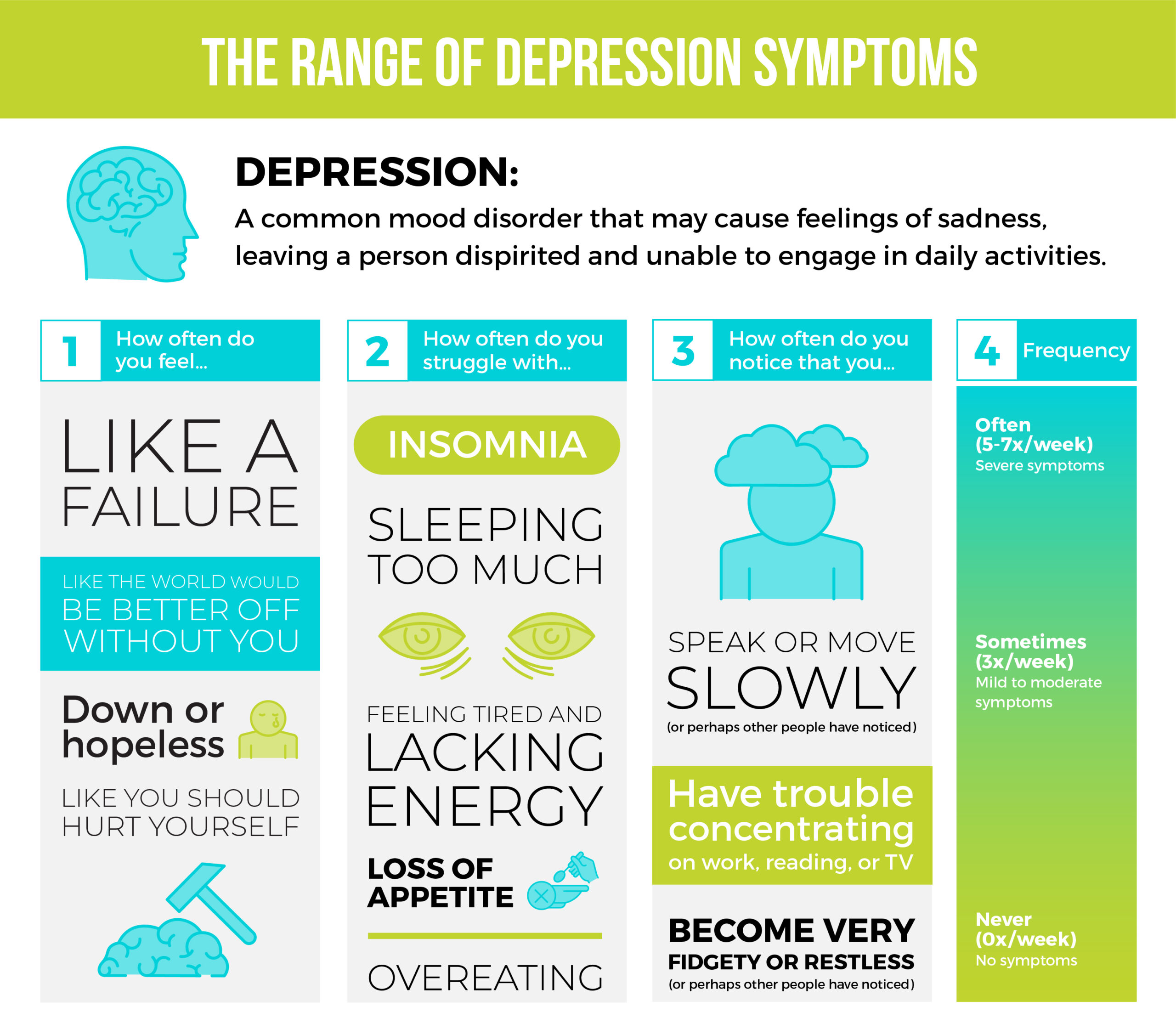
Depression – One of the most common mental health conditions, depression causes people to lose pleasure in life. More than just experiencing a day or two of sadness, for those suffering, the sad feelings don’t go away. They persist and interfere with everyday life causing a person to feel extremely tired, empty and hopeless, and in extreme cases, can even lead to thoughts of death or suicide.
Post-traumatic Stress Disorder (PTSD) – After going through a traumatic experience, it’s completely normal to go through emotions like fear, distress, helplessness, guilt, shame, anxiety or anger. With PTSD, those feelings don’t fade away, and the person feels stressed or frightened long after the trauma is over.
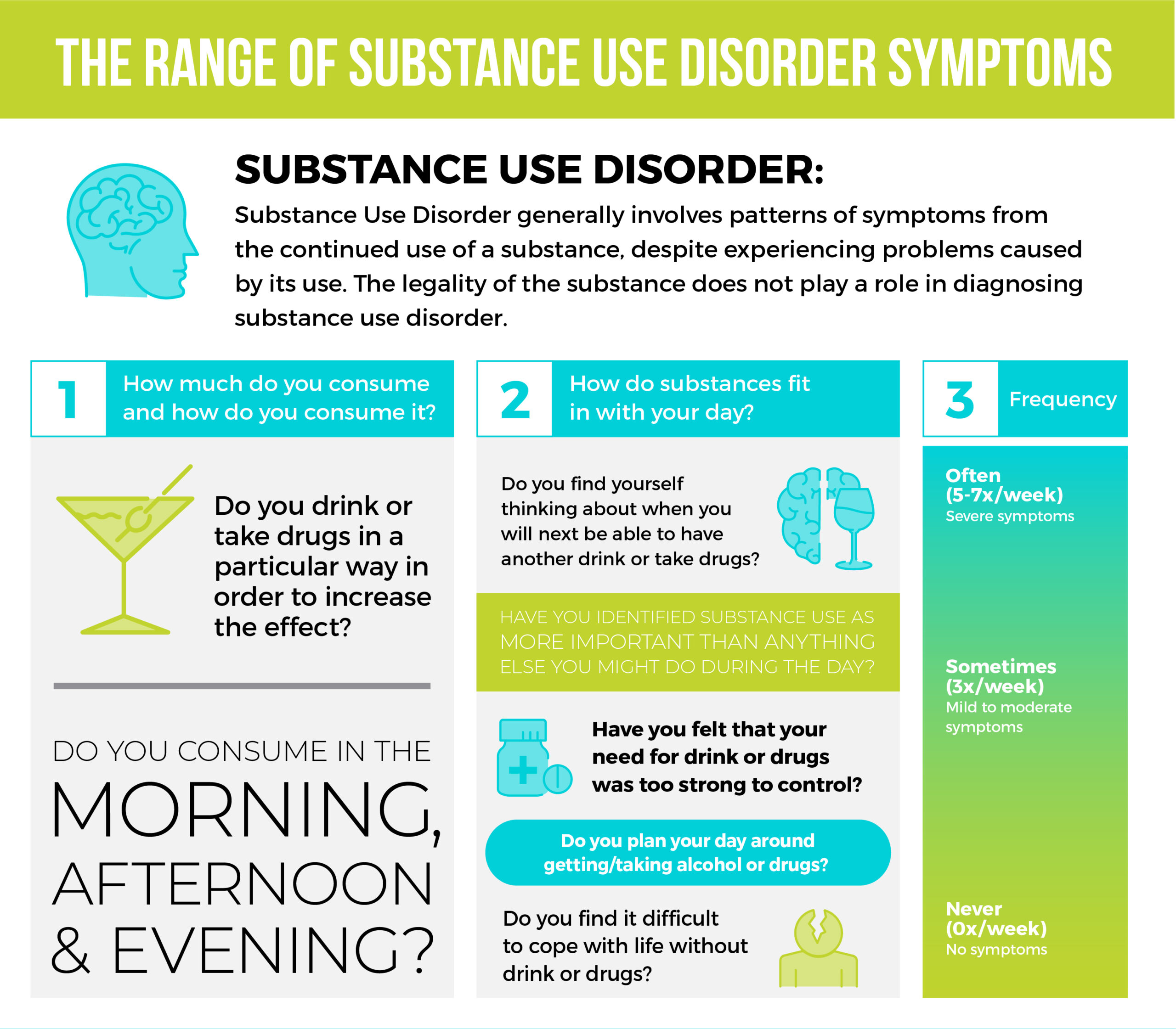
Addiction/Substance Use Disorder – For some people, the use of substances can become problematic and lead to dependence. Those suffering from substance abuse disorders have distorted thinking and behaviours causing them to have intense cravings and changes in personality. Often a person’s ability to function in day-to-day life or maintain valuable relationships becomes severely impaired.
Obsessive Compulsive Disorder (OCD) – This anxiety disorder is characterized by repetitive, uncontrollable, unwanted thoughts with irrational, excessive urges to do certain actions. These repetitive acts help relieve stress and anxiety brought on by an obsession as the person suffering believes that these rituals will help prevent something bad from happening.
Having a conversation about mental health
It can be difficult for someone to talk about their struggles with mental health, but creating a judgement-free zone and showing your support is a great way to get help them feel more comfortable and open up. However, it’s important to understand that this is an extremely touchy subject to broach and it can go sideways at the slightest turn. That’s why it is strongly advised that you seek a professional consultation before you initiate the discussion so you know what to say and how to say it. Read on for some tips to help you have a successful conversation.
Knowing when to start the conversation
You don’t need to be an expert to recognize when friends or loved ones need help, although there are a few signs to look out for. Please be advised that this is just a guide to help recognize some of the changes that may occur in those who are struggling with mental health.
Changes in appearance:
- Bloodshot or glassy eyes
- Unprofessional appearance or poor hygiene
- Unexplained injuries such as cuts, bruises, scrapes or marks
- Dramatic weight loss or gain
- Multiple physical ailments without obvious causes (like headaches, stomach ache, vague/ongoing aches and pains)
Changes in energy levels or mood:
- Exhaustion or fatigue from lack of sleep
- Loss of interest in pleasures of life
- Feeling excessively sad or low
- Unpredictable mood swings, including uncontrollable highs or extreme feelings of euphoria, irritability or aggression
- Inappropriate verbal or emotional responses and behaviours
- Relationship disharmony (e.g. how they speak about loved ones)
- Thoughts of suicide
- Changes in sex drive
Changes in function
- Decline in effort or performance (e.g. increasingly ordering takeout or not cleaning their spaces)
- Changes in sleeping habits
- Excessive worrying or fear
- Noticeable errors in judgement
- Decline in punctuality
- Inexplicable absences in personal and work life
- Difficulty perceiving reality (delusions or hallucinations)
- Avoiding friends and social activities
- Problems concentrating or learning
- Inability to carry out daily activities or handle daily problems and stress
Ask yourself: are you the right person to start this conversation?
An important thing to remember is that being supportive doesn’t mean it’s your duty to “fix” the person struggling. As you know, mental health is complicated and the solutions don’t happen overnight. If you’re comfortable being their sounding board, helping them navigate resources and providing encouragement, you’re already off to a great start.
Ask yourself these 3 questions:
Do they trust you? One of the biggest fears the person suffering has to overcome is having others find out about their mental illness. That’s why they rarely initiate mental health conversations themselves and will likely only talk about it with someone they know and trust.
Can you speak calmly and rationally? What they need most right now is patience and understanding. If you believe that you can provide that for them without reacting negatively to whatever they have to say, you could be the right person to have the conversation.
Can you be non-judgemental or accusatory? Mental health issues don’t just affect the person struggling, but their friends and family as well. If you think you’ll have a hard time holding your strong emotions in, the conversation should probably be had by someone else.
Tips on how to start the conversation about mental health
The most important thing you can do before beginning a conversation with a loved one about their mental health is to get rid of your expectations. Remember, while it can be a big relief for someone to share their personal experiences with mental illness, these struggles often require more than one conversation.
For starters, pick a quiet place to talk without distractions, like a park or a beach. You could also grab a snack and take a drive (which is a great solution if you feel the person you’re talking to wants to avoid eye contact). Lastly, ensure that they are not manic or under the influence when you have the conversation or it could backfire.
Here are some questions/phrases to help get you started:
- “How have you been feeling lately? I’ve noticed that you’ve seemed (insert adjective: distant/overwhelmed/tired).”
- “Is there anything I can do for you right now? What do you think you need at this moment in time?”
- “What do you usually do to cope with stress? Have you found anything that works well for you?”
- “I noticed you haven’t been around as much lately, is there anything you’d like to talk about?”
How to provide continuous support to those suffering
So you had the conversation with your loved one. They responded and are (thankfully) starting to get the mental health treatment they need. What do you do next?
Stay supportive. Continue to be their listening ear so they don’t feel isolated while going through treatment.
Stay in touch. If you don’t live with them, check in regularly. Offer to go grab a coffee or go for a walk so you can talk things out in a calm environment.
Stay curious. Don’t be afraid to ask how their treatment is going, just remember to always be tactful and compassionate when inquiring.
Stay vigilant. If you’re concerned that your loved one is at risk of harm or they’re talking about ending their life, this could be a medical emergency. Call 911 and stay calm until help arrives.
Stay aware: Continue to educate yourself and take note of helpful resources that you can offer to share with them. To find resources specific to your region, visit the Canadian Mental Health Association.
Conversational do’s and don’ts when addressing mental health
Ready to start the conversation? Here are a few tips on how to help someone struggling with mental health and avoid the pitfalls that can stop this important conversation in its tracks.
DO
Listen. Let them get all of their thoughts out without interrupting. After they’ve finished, then you can respond.
Ask them what they need. No matter what have they to say, take them seriously and don’t minimize their feelings.
Talk about options for support. Do your homework so you’re aware of the treatment options available and can help point your loved one in the right direction.
Remain calm at all times. Though some of the things they share may be worrisome, do your best to be a pillar of strength so they can get their feelings out.
DON’T
Judge or criticize. Insulting their emotions or actions doesn’t help and will only push them away.
Worry about having all the answers. Remember it’s your job to listen so you can help guide them towards getting the help they need. It’s not up to you to provide it. If you can, prepare yourself with some resources that can help, ahead of the conversation.
Force communication, lecture or try to fix the problem. While you understand how much of a relief it can be for someone to share, it’s not your job to get it out of them or try to solve it.
Use a confrontational approach to incite guilt or shame. Acting in this way will often push those who are struggling away as they will want to avoid feeling worse than they already do.
Mental health support on the go
Need some help remembering the tips you read here today? Download our useful infographic for a takeaway summary of this article, including tips on how to help support your loved one’s emotional well-being through their mental health struggles.
Be prepared for conversations surrounding mental health. Contact us today to learn how EHN can help.
EHN CAN HELP
Whether you’re an individual who needs help with your mental health or substance use disorder, a friend of someone struggling or you’re an employer with employees who need help—we’re here for you. Call us 24/7 at one of the numbers below to start a conversation about how we can help you.
- Bellwood (Toronto, ON): 866-281-3012
- Edgewood (Vancouver Island, BC): 604-210-8713
- Ledgehill (Lawrencetown, NS): 866-419-4483
- Sandstone (Calgary, AB): 866-295-8981
- Gateway (Peterborough, Ontario): 705-874-2000
- Nouveau Depart (Montreal, Quebec): 866-738-5572
- EHN Online: 866-345-8192
This Mental Illness Awareness Week, do what you can to acknowledge the realities of mental health disorders. Reach out—check in on friends, educate yourself, start valuable conversations. You may be surprised at how great of an impact it can make for someone struggling.
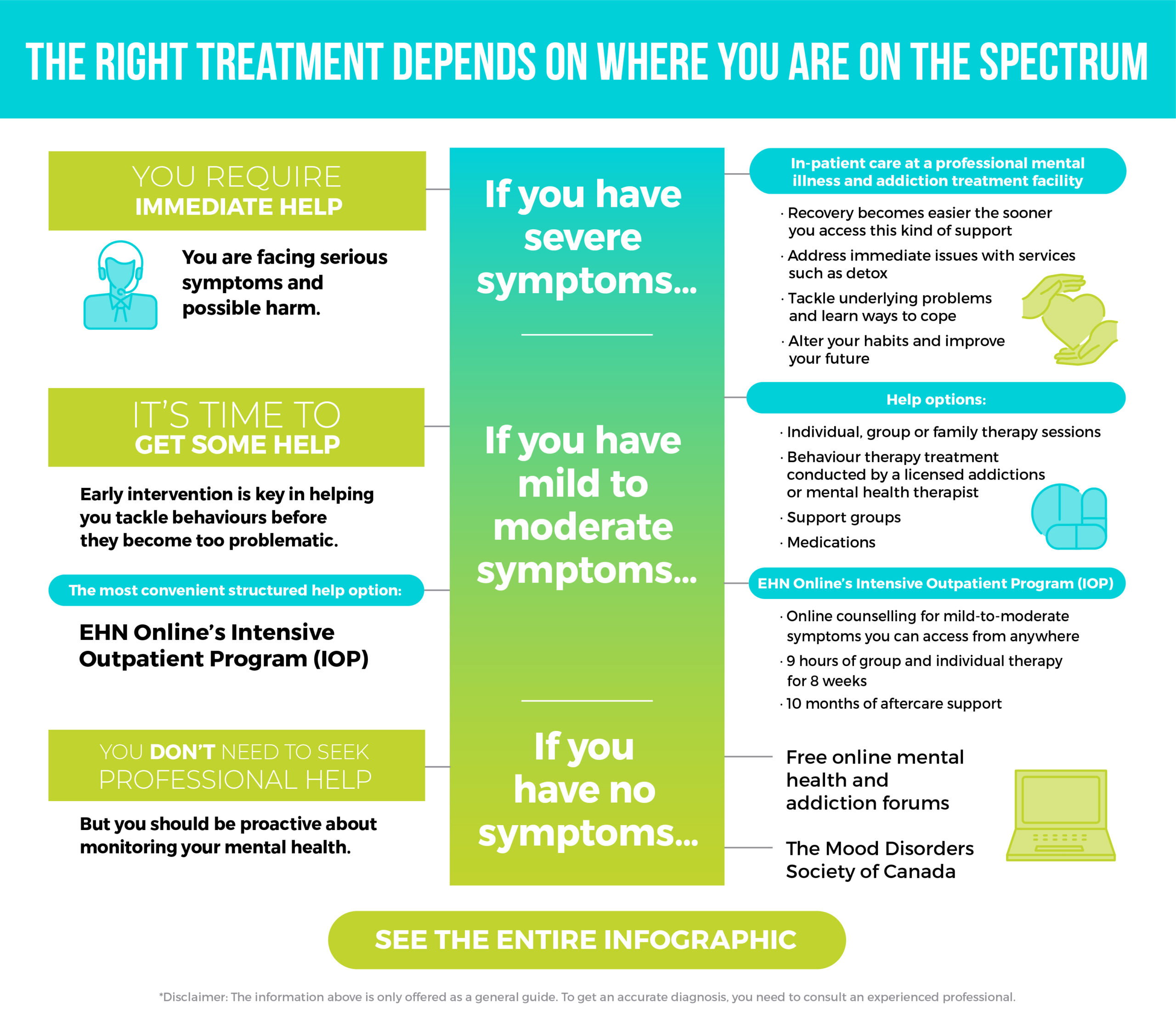
 When we think of mental health challenges and addiction issues, we probably think of extremes. Sober or alcoholic. Healthy or not. Panic attacks where you’re bed-bound for days. Liver problems from excessive drinking.
When we think of mental health challenges and addiction issues, we probably think of extremes. Sober or alcoholic. Healthy or not. Panic attacks where you’re bed-bound for days. Liver problems from excessive drinking.