Does online rehab really work?
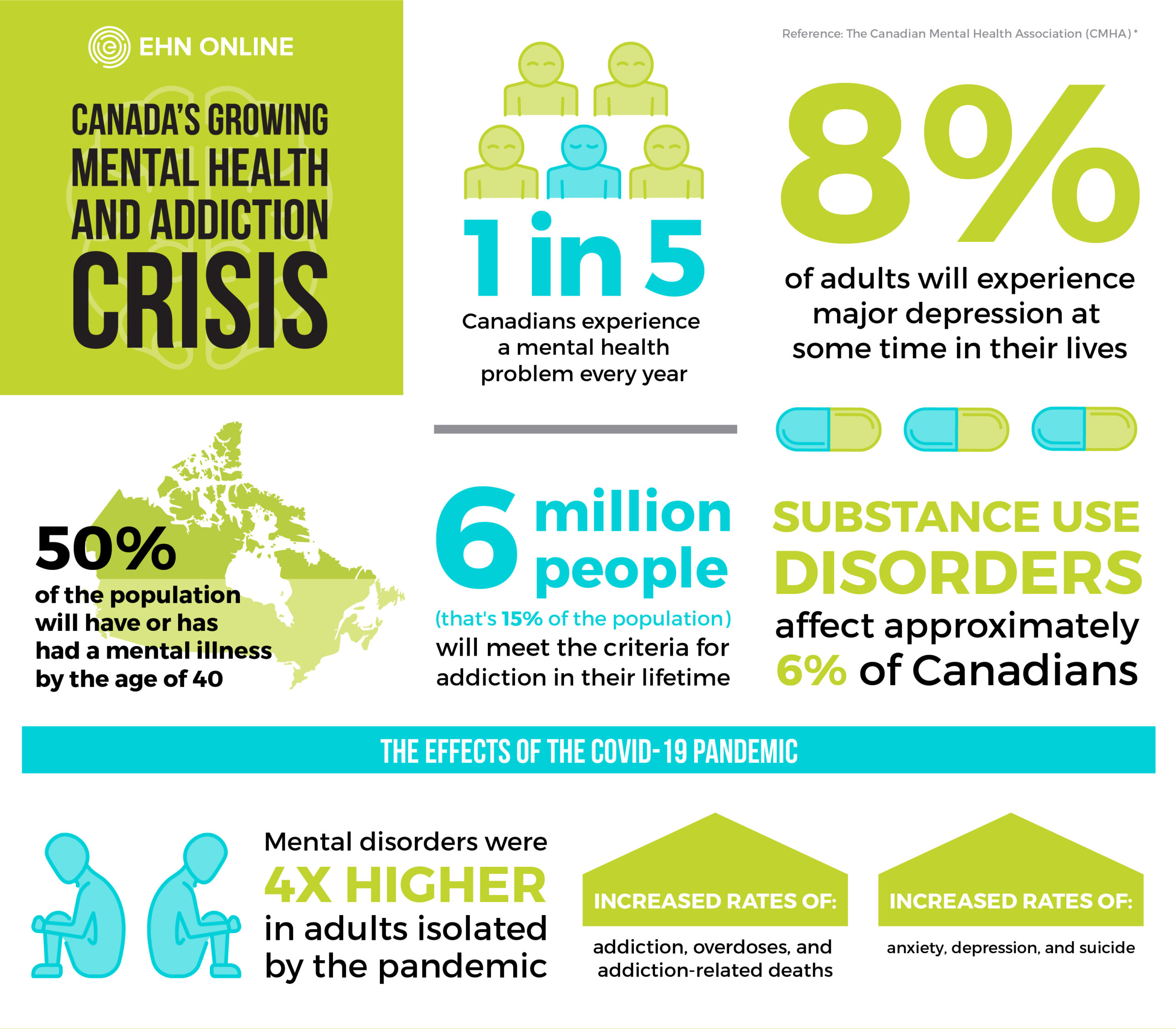
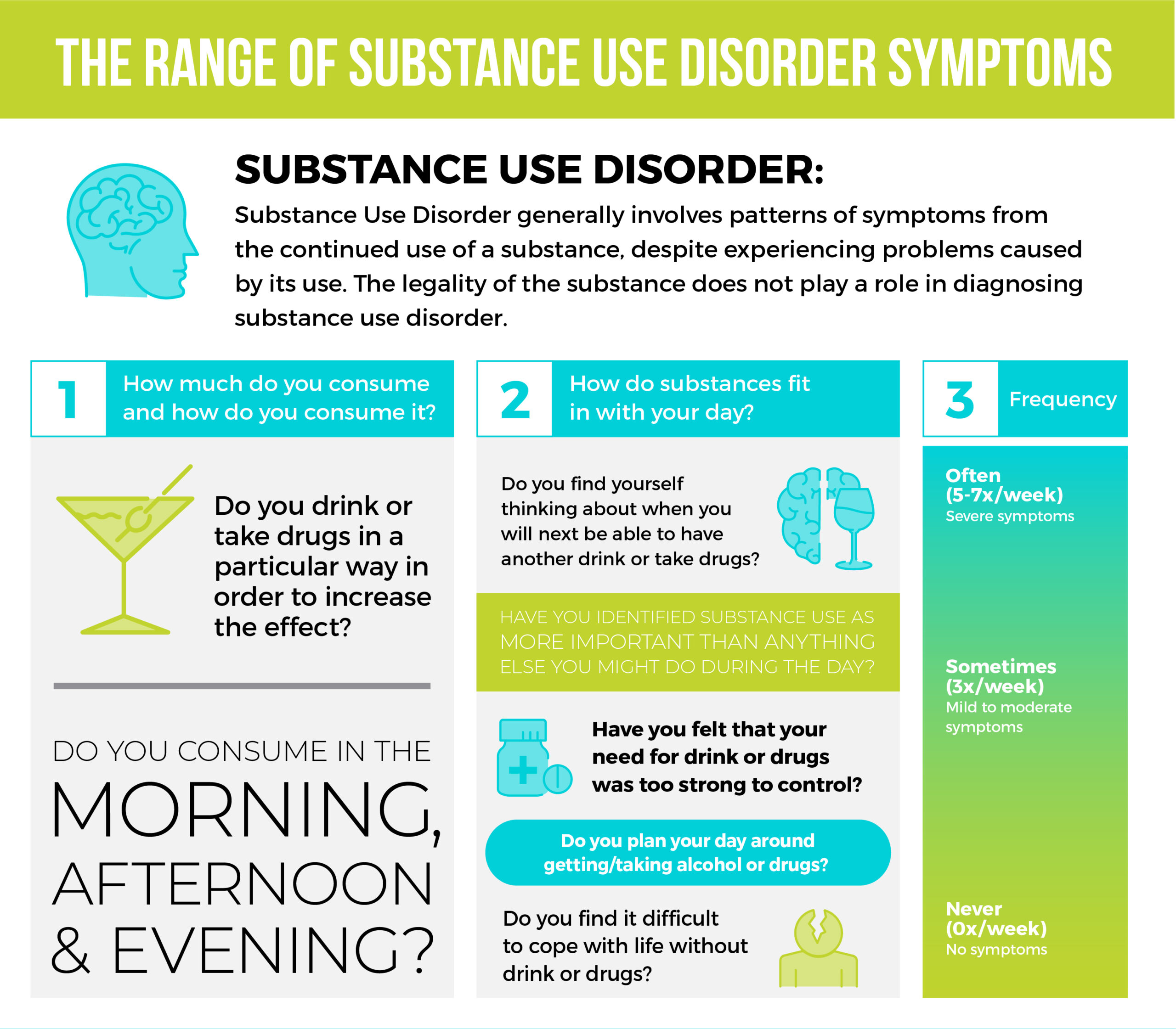
The ongoing stress and uncertainty of COVID-19 has led to an increased demand for mental health services in Canada. While we often think of mental health issues like anxiety and depression as the predominant conditions people are challenged by at this time, we are also facing a public health crisis with increasing opioid, alcohol and stimulant addictions. More than ever, people need varied and accessible treatment options to recover from addictions.
One form of service filling this need is virtual or online treatment. Online programs make recovery more affordable and accessible – but are they effective in treating addiction?
What makes rehab effective?
Within the different types of treatment options that exist, there are common factors that make a rehab program effective. An effective rehabilitation program will focus not only on the individual’s substance use, but also on coping strategies, interpersonal relationships, and other important areas of functioning.1 While the definition of success may vary from one program to another, effective treatment should always include a few common results.
A person receiving effective addiction treatment should demonstrate some of the following:
- Reduced amount and frequency of substance use, including longer gaps between relapses
- Improved employment or education status and attendance
- Improved physical health, indicated by fewer medical visits
- Improved mental health, indicated by improved mood, personality traits and behaviors
- Improved relationships with friends, family, and others2
A good program should ultimately help you reach and maintain sobriety, using the coping skills you develop while in treatment. As a result, other areas of your life should also improve.
Differences and similarities between virtual and in person
Some elements of in person and virtual rehab are very similar while others can be slightly different. Both are highlighted below.
Differences
Accessibility
One of the main differences between the two are accessibility. With an online program, you can seek help no matter where you or the program are based. With convenience and location removed from the equation, you can focus on the program and specialities best suited to your individual needs. You also don’t have to worry about factors like weather or access to transportation.
Travel and Time Commitment
Because there is no travel time for online addiction treatment, another thing that differs is your time commitment. You no longer need to factor in the time it takes to commute to and from your program. It is also worth noting that online programs may be very structured, but they also give you the freedom to recover from home while you continue to work or tend to family commitments.
Perceived Vulnerability
As with any recovery program, there is always a perceived vulnerability involved in trying something new and for some, anonymity can be an important aspect of a program. Because you can participate on a virtual platform further away from your home, there is less chance of running into someone in your program you know, which can provide a sense of greater freedom to be vulnerable. You also don’t run the risk of seeing someone you know in a parking lot or near the location of your program, which can remove a lot of anxiety involved in seeking and getting help.
Affordability
It is also worth noting that there can be a difference in cost. Because you are not living in a facility, online programs are not as costly as in-person rehab. In addition, you don’t have to worry about expenses like childcare or gas, as you are recovering from home.
Similarities
Personal Connections
Like in person rehab, virtual programs allow you to make personal connections with those in your program. Not only can you connect with the professional leading the program, but there is also the opportunity to connect with peers as you would in person. Group sessions and shared experiences, whether online or in person, have therapeutic benefits and encourage the creation of emotional connections with others.
Crisis Response
Both types of programs also offer interventions in case of an emergency. Those trained to run in person and online sessions know how to spot someone in crisis by reading their facial expressions and physical cues. Many programs also offer apps, where a person can self-report if they need immediate assistance.
Efficacy
For people experiencing mild-to-moderate addiction symptoms, online treatment can be equally, if not more, effective than in-person rehab. With the right program, you can meet all the “efficacy qualifications” listed above, with the added benefit of being able to practice and encourage the skills and coping mechanisms you are learning in real time. One area of your life where you can practice this is in your relationships. When you are doing the work from home, you have the opportunity to discuss and repair relations with your family and friends.
Proven benefits of online rehab
Online rehab offers many benefits, especially for someone with mild to moderate addiction issues. As mentioned above, virtual programs are often more accessible, especially for those who live in remote areas and would not have help close by otherwise.
While it would be great if everyone could occasionally take a break from their everyday lives to work on their wellness, for many, that is simply not possible. Online programs allow you to continue to live at home and go to work if you need to.
When your life has not been uprooted, you can recover without worrying about how much time you are away from home for, what it is you might be missing, or how soon you have to re-enter your day-to-day routine. It also helps you to recover without removing some of the stressors in your daily life, which gives you the opportunity to apply new coping skills in real-time, something you might not necessarily get to practice in a residential treatment program.
There is evidence that shows that those with social anxiety often do better in online settings as they are less concerned about encountering others face-to-face.3 This can make it easier to open up and express the challenges you are facing.
It is worth noting that even though they are online, these programs are structured. They have set times and specific activities or exercises that are designed to keep you on track and give you better support overall.
How EHN Online’s program sets you up for sobriety
EHN Online’s addiction recovery program has several benefits to help set participants up for success. The Substance Use Disorder Intensive Outpatient Program (IOP) is structured to provide an eight-week intensive rehabilitation course that provides a wide variety of education and skills to help participants regain control over their cravings, habits, and lives. Each week will include nine hours of treatment time composed of individual and group therapy, as well as psychoeducation about substance addiction and skill building.
Following the eight weeks of intensive care, participants have access to 10 months of aftercare, keeping up with progress tracking on the Wagon app, and meeting with a group once per week. This will encourage maintenance of positive habits and beneficial skills, while continuing the opportunity to build a strong support network of individuals with similar experiences and hardships.
If your loved ones are looking for better ways to support you, EHN’s IOP also offers a Family program as part of the package, so that loved ones can also receive advice and access better tools to aid in long-term recovery.
EHN Online’s substance use disorder program provides all the benefits of virtual rehab, such as accessibility and structure, while also making treatment affordable and providing the chance to work on challenges, skills and relationships in real time.
Most importantly, EHN Online’s virtual program is one that works. While there is no one “right” way to receive treatment, as the effectiveness of each setting and treatment approach is dependent on you and your unique situation, online rehab can be a sustainable and helpful option to consider.
How to access an online rehab program
If you have mild to moderate addition symptoms and believe online rehab may suit your needs, then don’t hesitate to call us. Our consultations are free and there are no wait times for enrolment. Book an assessment and see if this program is right for you.
It is always a good time to get started, so give us a call today!
Be prepared for conversations surrounding mental health. Contact us today to learn how EHN can help.
References
- Administration (US), S. A. and M. H. S., & General (US), O. of the S. (2016). Early Intervention, Treatment, and Management of Substance Use Disorders. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. US Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424859/
- May 28, E. S. L. U. & 2021. (n.d.). How to Find Effective Drug Rehab Programs? How to Evaluate American Addiction Centers. Retrieved September 6, 2021, from https://americanaddictioncenters.org/rehab-guide/effective
- McCall, H. C., Helgadottir, F. D., Menzies, R. G., Hadjistavropoulos, H. D., & Chen, F. S. (2019). Evaluating a Web-Based Social Anxiety Intervention Among Community Users: Analysis of Real-World Data. Journal of Medical Internet Research, 21(1), e11566. https://doi.org/10.2196/11566
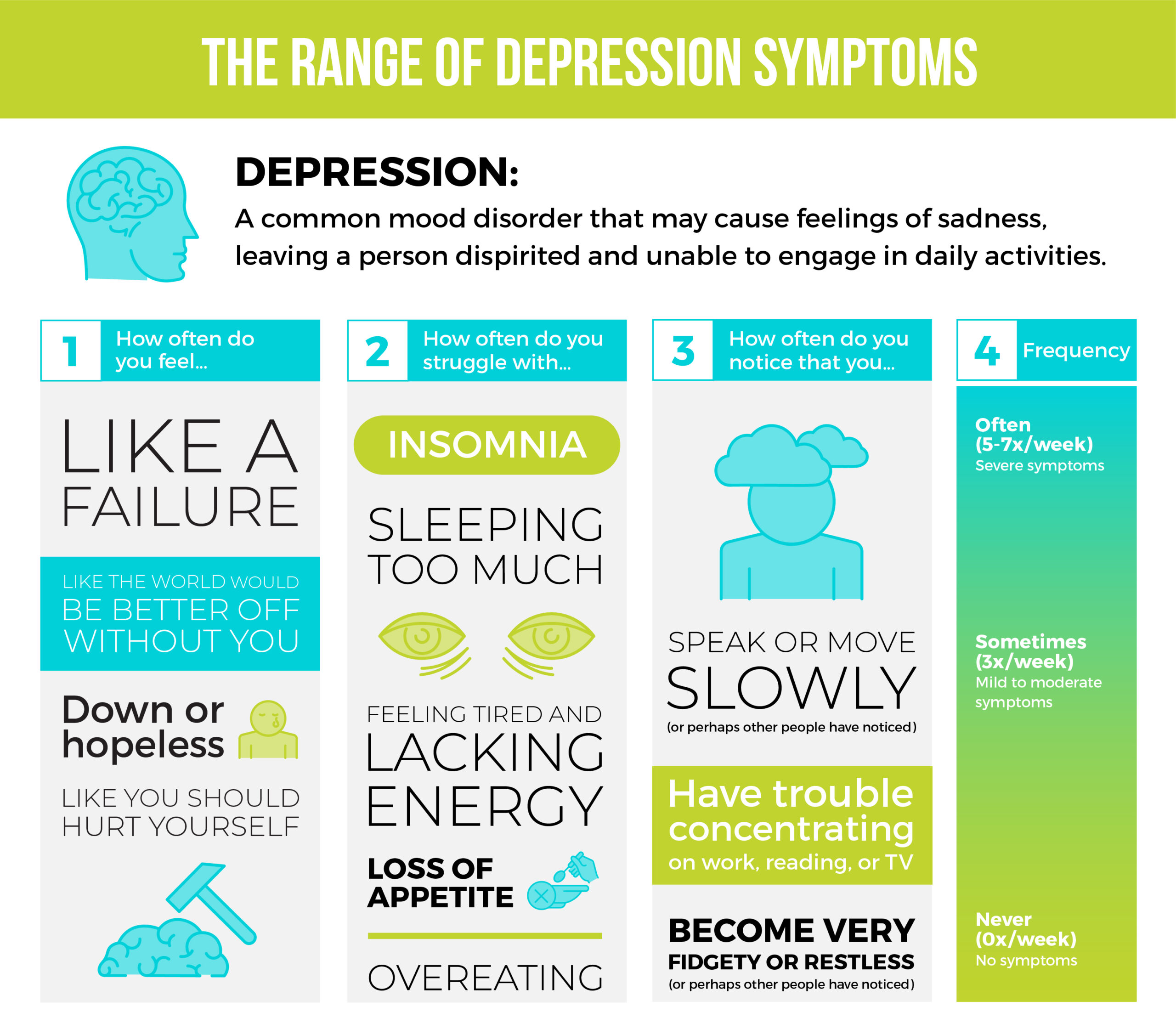
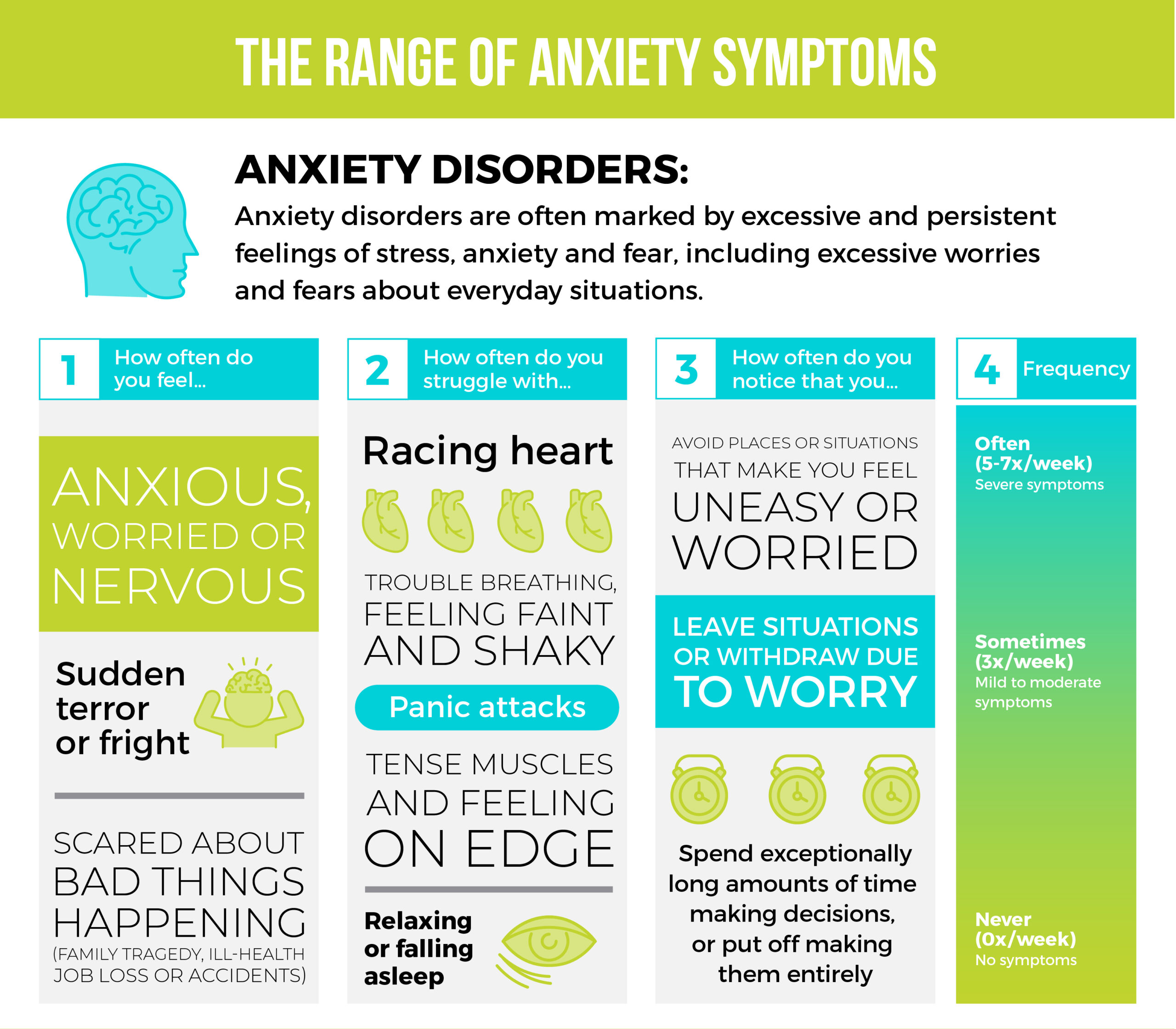
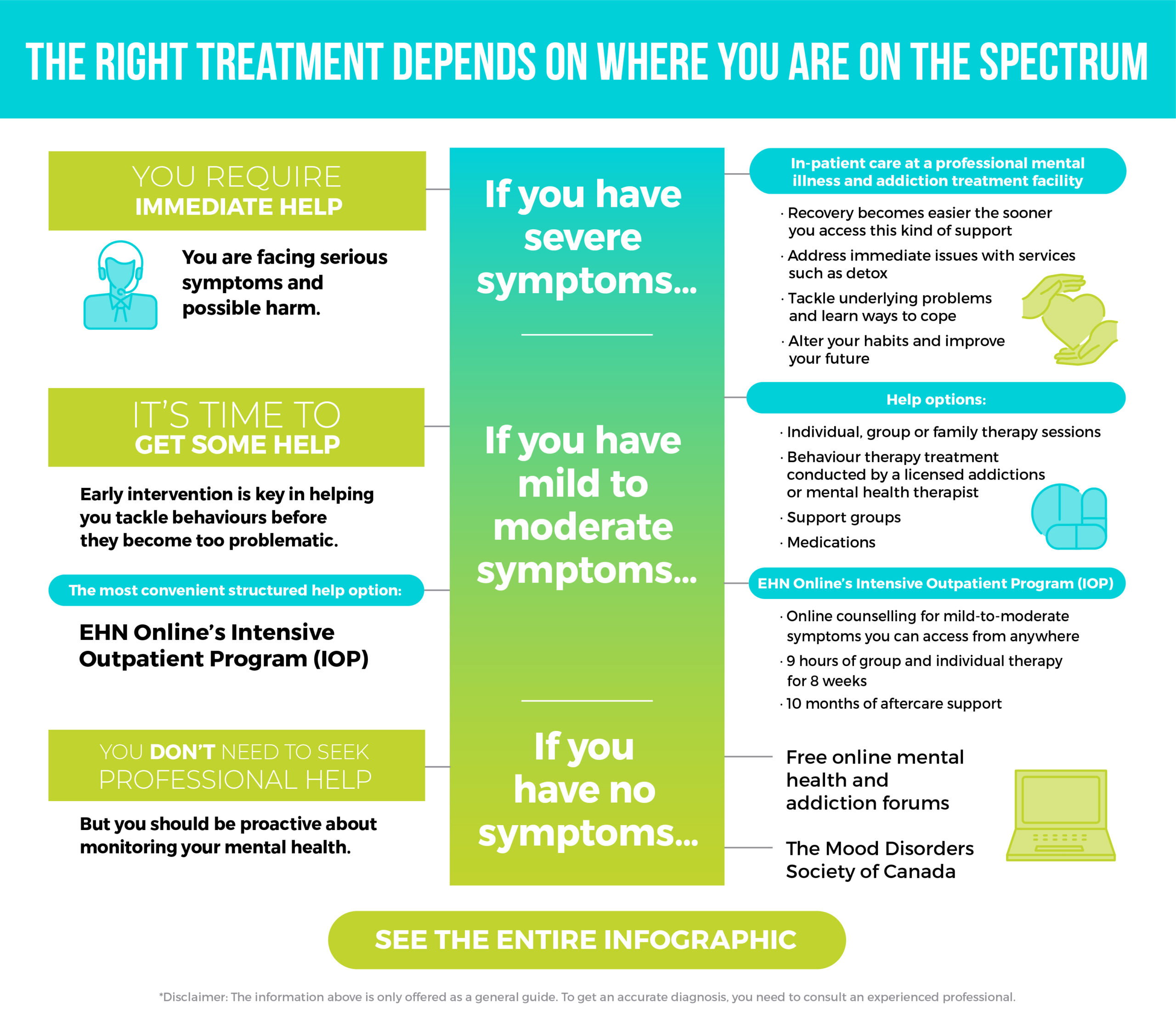
 When we think of mental health challenges and addiction issues, we probably think of extremes. Sober or alcoholic. Healthy or not. Panic attacks where you’re bed-bound for days. Liver problems from excessive drinking.
When we think of mental health challenges and addiction issues, we probably think of extremes. Sober or alcoholic. Healthy or not. Panic attacks where you’re bed-bound for days. Liver problems from excessive drinking.